Understanding Biofilm: The Hidden Barrier to Healing Chronic Wounds
Understanding Biofilm in Chronic Wounds
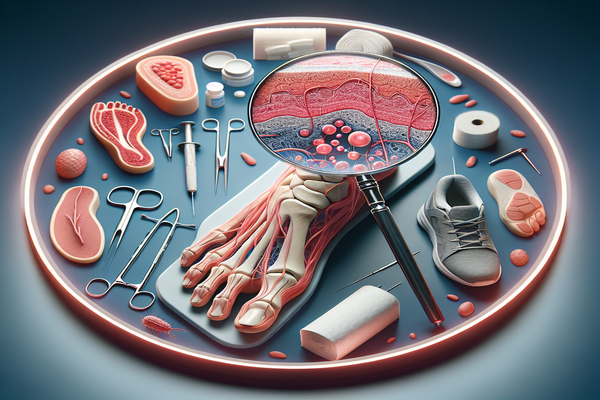
At American Surgeons Group, located in the South Chicago Suburbs, we understand that healing chronic wounds can be complex. One significant factor that hinders effective healing is the presence of biofilm—a slimy layer of bacteria that can form on various surfaces, including wounds. In this article, we will explore what biofilm is, how it affects chronic wounds, and what can be done to treat it.
What is Biofilm?
Biofilm is a structured community of microorganisms, including bacteria, that adhere to surfaces and encase themselves in a self-produced protective matrix. This matrix can be composed of polysaccharides, proteins, and nucleic acids, making it very resilient against the host’s immune response and antibiotics.
How Does Biofilm Affect Wound Healing?
The presence of biofilm in chronic wounds creates multiple challenges:
- Impeded Immune Response: The protective matrix of biofilm can shield bacteria from the body’s immune cells, preventing effective healing.
- Antibiotic Resistance: Bacteria within biofilms often exhibit resistance to antibiotics, making it difficult to eradicate the infection.
- Chronic Inflammation: The immune system’s ongoing attempts to combat biofilm can lead to persistent inflammation, further delaying the healing process.
- Delayed Healing: The combination of these factors can result in wounds that fail to progress through the natural healing stages.
What Causes Biofilm Formation in Wounds?
Several factors contribute to biofilm formation in chronic wounds, including:
- Moisture Levels: Excessive moisture, often seen in wounds not adequately managed, can promote biofilm growth.
- Presence of Foreign Bodies: Prosthetic devices, sutures, or other materials can serve as surfaces for biofilm establishment.
- Chronic Conditions: Diabetes, venous insufficiency, and peripheral arterial disease increase the likelihood of chronic wounds developing biofilms.
- Poor Circulation: Insufficient blood flow hampers healing and can encourage the growth of bacteria.
How Can I Treat Biofilm in Chronic Wounds?
Addressing biofilm effectively requires a comprehensive approach to wound care. Here are key strategies:
- Debridement: Removing non-viable tissue and biofilm can enhance healing. This is often performed by a healthcare professional.
- Antimicrobial Dressings: These can help control bacterial growth and disrupt biofilm formation.
- Regular Monitoring: Frequent evaluations by a podiatrist can help in adapting treatment plans as necessary.
- Advanced Therapies: Treatment options such as negative pressure wound therapy (NPWT) or growth factor therapy may be recommended based on your specific needs.
- Systemic Treatment: In some cases, antibiotics effective against biofilm-forming bacteria may be indicated, ideally guided by a culture and sensitivity test.
What Foot Conditions Are Most Likely to Involve Biofilm?
Biofilm-related chronic wounds can stem from various foot conditions, such as:
- Diabetic Foot Ulcers: Common in individuals with diabetes, these ulcers can become infected and complicated by biofilm.
- Venous Ulcers: Resulting from poor blood flow, these ulcers can also fall victim to biofilm formation.
- Pressure Ulcers: Often arising from immobility, these ulcers can be challenging to heal when biofilm is present.
- Fungal Infections: Conditions like athlete's foot can lead to secondary infections, further complicating wound healing.
Can Biofilm Be Prevented?
While complete prevention of biofilm formation may not be feasible, certain measures can reduce the risk:
- Maintain Proper Hygiene: Regularly cleaning and caring for your feet can help keep wounds clean.
- Moisture Control: Keeping the wound environment balanced—neither too moist nor too dry—can inhibit biofilm development.
- Address Chronic Conditions: Managing diabetes, circulation issues, or other underlying health problems is crucial for reducing wound risk.
- Regular Check-ups: Routine visits with a podiatrist can ensure any potential issues are caught early.
Frequently Asked Questions (FAQ)
1. How do I know if my wound has a biofilm?
Signs may include persistent infection, non-healing wounds, increased pain, or the presence of a foul odor. Consultation with a podiatrist is essential for proper diagnosis.
2. Is biofilm visible on my skin?
Biofilm is typically not visible; however, signs of infection or chronic non-healing wounds suggest its presence.
3. How long does it take to treat a biofilm infection?
Treatment duration varies based on the severity of the infected wound and individual health factors, often requiring weeks to months.
4. Can I manage chronic wounds at home?
While initial care can often be managed at home, professional evaluation and treatment by a podiatrist are crucial for chronic wounds, especially if biofilm is suspected.
5. When should I see a podiatrist for a wound?
If your wound does not show signs of healing within a few weeks or worsens, it’s vital to consult a podiatrist at American Surgeons Group.
Conclusion
Biofilm is a crucial barrier in the healing of chronic wounds, including diabetic foot ulcers and venous ulcers. Understanding biofilm and its implications on wound healing can empower patients to take proactive steps in their care. At American Surgeons Group in the South Chicago Suburbs, we’re here to provide expert care and support for your foot health. If you have concerns about chronic wounds or biofilm, book an appointment today to receive personalized treatment options that can lead you toward healing.
